Mark Lightbody
MFT NHS Foundation Trust (Withington Community Hospital)
Background
As part of the Scientist Training Programme (STP), trainees have the opportunity to spend up to six weeks completing an elective placement in an area of their choice. For my elective placement I decided to spend five weeks in Guatemala City working for a hearing, balance and phonetic training clinic called CEDAF. I decided to spend my elective in Guatemala because I wanted to gain first-hand experience in a healthcare system unsupported by a national health service and where many people cannot afford private health insurance. I also wanted to understand how healthcare is delivered and maintained in a country with a poorly financed health system and where poverty, illiteracy and other social factors act as obstacles in healthcare provision.
The clinic I visited was established and is run by Dr Patricia Castellanos de Munoz who is the only licenced Audiologist in the country. Dr Castellanos has faced the struggles of being a female clinician, entrepreneur and business woman in the male-dominated workforce of Guatemala. Her hard work in hospitals, clinics, schools and foundations throughout Guatemala City along with her perseverance to develop an independent Audiology service have led her to become a leading expert in Audiology throughout Latin America.

Dr Castellanos established CEDAF as a private clinic offering audiological care to those with the means to pay for healthcare; however, one of Dr Castellanos’ initial aims was to grow her business to support people unable to afford audiological services. In order to achieve this, she set up a foundation in 2009 called Sonrisas que Escuchan (which translates from Spanish as Smiles that Listen) to provide an audiology service to those that cannot afford it.
The foundation provides audiological care to people of all ages with a focus on developing neonatal and school hearing screening programmes to help children with hearing loss. Children who fail the screen are referred to the clinic at CEDAF to have free diagnostic audiological tests and to discuss hearing aid provision. Those requiring hearing aids are encouraged to use them and the cost of the hearing aids and their maintenance is subsidised by the foundation. With special thanks to Oticon, I was able to take over 600 used hearing aids with me for the charity to use. I have been kept updated about their use and Dr Castellanos assures me that they have been an enormous help for her foundation.
Working with the foundation in public hospitals and schools and with the CEDAF team at the private clinic provided me with eye-opening and invaluable experiences which I will value throughout my career in audiology.
Newborn hearing screen
There is particular disparity in the provision of healthcare in Guatemala due the extreme difference in social status throughout the country. Over 50% of the population live below the poverty line with millions unable to pay for private health insurance and having to rely on the poorly funded public health service. However, much of the treatment available in the public hospitals is only available to those that are employed with the unemployed only able to access the most basic healthcare. Unfortunately, this encompasses much of the population due to high levels on unemployment in the country.
The role of Sonrisas que Escuchan is to remove this healthcare bias and provide an Audiology service to those that need it most. To try and achieve this, the foundation has successfully set-up the neonatal hearing screening programme in three public hospitals. Due to limited funding and resources, however, the foundation can only provide screening once per week at each location which makes it difficult to reach all those that need the service.
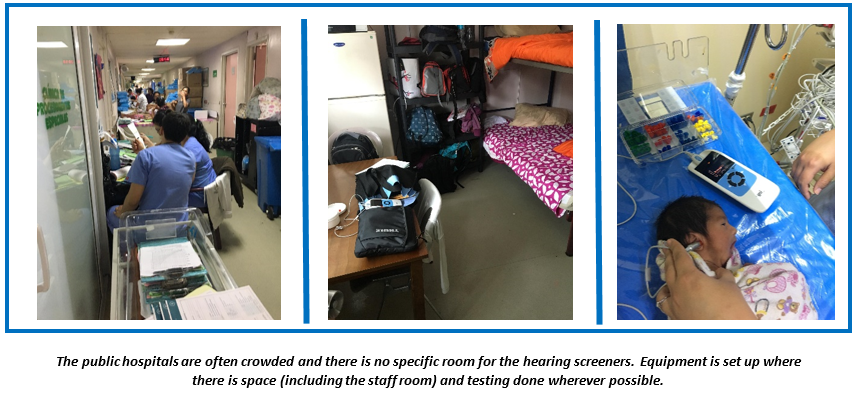
This was very interesting for me to experience as the foundation adopts a very different approach to the UK screening programme. In Guatemala City it is simply not possible to test the hearing of all babies at birth due to a lack of trained screeners and equipment. Instead, the babies most at risk of hearing loss are screened, which included those born premature, those that have contracted sepsis and those in intensive care.
For those babies who failed the screen, a referral was made to CEDAF for further assessment regardless of the family’s ability to pay for the service. The family was invited to the audiology clinic with travel and accommodation provided for those that needed it. Those diagnosed with permanent hearing loss were then applicable to receive full audiological care including hearing aid provision and speech therapy. Although not a faultless system, the best efforts were made to provide a fair and comprehensive service to those that needed it.
Training of hearing screener
During my placement, the sole hearing screener decided to leave her role which meant a new screener had to be trained. This was a great opportunity for me to provide technical advice to ensure the safe and effective delivery of services in line with good scientific practice. I was able to advise the new screener on how to use the Otoacoustic Emissions (OAE) equipment, which is a screening device to test cochlear function. The equipment is fairly simple to use but an effective technique has to be adopted and an adequate noise environment has to be established to produce results. I demonstrated the best way to conduct OAEs and helped provide an idea of how many babies could be tested in the time available. The paediatric doctors had unrealistic expectations of how many tests could be completed in one session, so it was important to train the screener to conduct high quality testing rather than a high quantity of tests.

Furthermore, I was able to help her understand hearing loss risk factors in neonates and which babies she should prioritised for screening. This helped the new screener gain confidence in understanding her capabilities, limitations and how to make the service as efficient as possible.
School screening
Participating in the school hearing screening programme was a good opportunity to develop my skills in clinical leadership by working with a new clinical team in a different working environment away from the hospital setting. The school hearing screening programme that has been developed by Sonrisas que Escuchan is an important intervention to identify pre-school aged children with hearing loss. Education is only provided by the government up to elementary level and it is a challenge to encourage families to continue their child’s education instead of allowing them to work to support the family economically. Children with hearing loss are more likely to struggle at school and more likely to leave education earlier than their peers.
The foundation has established the school screen in Guatemala City and is now focused on developing the service throughout the country. I had the opportunity to participate in the school screen in the town of Santiago in the Solola province. The clinical team at this location consisted of two audiological technicians who had been trained in otoscopy, basic audiometry and ear cleaning. Understanding their abilities and proficiency in audiology was important for me to determine my role within their team and to provide advice on their practice. This was an interesting opportunity during the placement because there were many aural abnormalities that I was unfamiliar with but were common for the technicians to encounter. This was most likely due to the differences in cleanliness and hygiene standards of the children and their families in Guatemala compared to those I am used to seeing in the UK.
Networking with other foundations
I was extremely proud to be able to work with Sonrisas que Escuchan and provide as much advice and assistance as possible. One of Dr Castellanos’ aims for the foundation is to network with other non-government organisations (NGOs) to provide the most comprehensive healthcare possible to those unable to pay for or access it.
Discussions with Dr Castellanos gave me a clear understanding of the importance in networking with other NGOs to help patients and promote hearing care. During my placement I was able to network with other young professionals volunteering their skills to help NGOs. By doing this I managed to establish a connection with a foundation called TessUnlimited that provided surgery and care for people with cleft lip and cleft palate.

Children with cleft lip and palate are known to suffer from glue ear more than their peers. For this reason, children in the UK with cleft lip and palate have regular hearing tests. Many of them also require speech therapy and must be able to hear well for this to be effective. The healthcare providers at TessUnlimited were unaware of audiological services in Guatemala to test their patients’ hearing. I was able to inform them of the services offered by Sonrisas que Escuchan and a meeting was set up between the board of directors at TessUnlimited and Dr Castellanos.
The meeting was successful, and discussions are now underway with an ENT doctor who will hopefully provide grommets for the children with cleft suffering from recurrent glue ear. Sonrisas que Escuchan have also been able to offer advice on ear and hearing care and hopefully can secure funds to provide screening equipment and training for TessUnlimited staff to test their patients for hearing loss. I feel that this was an excellent opportunity for me to act as an ambassador for the Healthcare Science community.
Conclusion
It was interesting for me to learn about working in the healthcare system in Guatemala and it changed my perspective of the work provided by healthcare professionals in this setting. Before working with Sonrisas que Escuchan, I had considered that audiological care would be provided by the foundation to anyone requesting it. However, Dr Castellanos explained and demonstrated to me that it was worthless providing hearing tests/diagnoses in communities where follow-up treatment could not be sustained. She also had to work within the budget of her foundation and taught me how to prioritise cases. By setting out clear business strategies and aims for her foundation, Dr Castellanos is able to decide whether or not her foundation can support new projects around the country. If the project is not in line with the ethos of her foundation, then she is not able to offer support as it may have a detrimental effect on one of her other projects.
This placement also challenged my current thinking of audiology service provision. Practicing in the UK has taught me to identify which test neonates require (OAE or ABR) if they fail their hearing screen. In Guatemala, however, I had to decide which babies received the hearing screen based on hearing loss risk factors. This was an excellent opportunity to consolidate my knowledge in childhood hearing loss. In addition, my thought process around paediatric follow-up appointments was challenged as I take it for granted that parents will bring their children to hospital appointments in the UK. This is not the case in Guatemala, and it adds an extra component to the role of the audiologist when they have to focus considerable amounts of time and effort towards encouraging patients to attend appointments and educating them on hearing loss.
I feel that the skills I learned from Dr Castellanos and her team were particularly useful when I returned to the UK to carrying out my research project into the viability of group hearing aid appointments for my MSc in Neurosensory Science (Audiology). The lessons I learned about leadership and communication were integral for me implementing group hearing aid fitting appointments into my department when working with patients, peers and colleagues. The elective placement was also an excellent opportunity for me to identify areas of weakness and strength in my clinical practice and use this information to focus my training in a direction that ultimately made me a better Clinical Scientist.